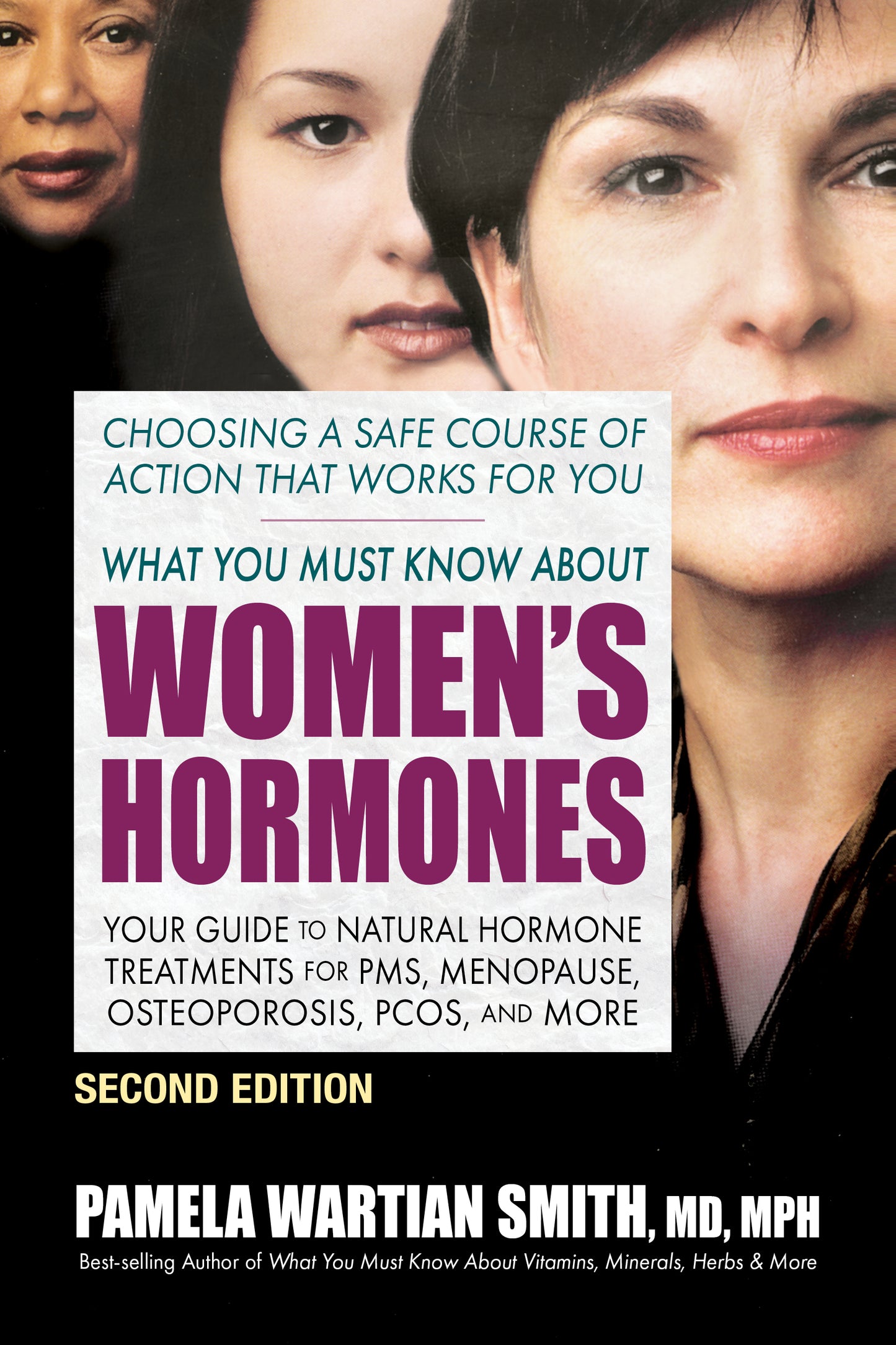
*** OVER 85,000 COPIES SOLD ***
Hormonal imbalances can occur at any age—before, during, or after menopause. The reasons for these imbalances vary widely, and can include heredity, environment, nutrition, and aging. While most hormone-related problems are associated with menopause, the fact is that fluctuating hormonal levels can also cause a variety of other conditions; and for some women, the effects can be truly debilitating. In this new and expanded edition of What You Must Know About Women’s Hormones, bestselling author Dr. Pamela Wartian Smith has provided a clear and concise guide to the treatments of hormonal irregularities without the health risks associated with standard hormone replacement therapy.
This book is divided into three parts. Part I describes the body’s own hormones, looking at their functions and the different side effects that can occur if these hormones are not at optimal levels. Part II focuses on the most common problems that arise from hormonal imbalances, such as PMS, hot flashes, postpartum depression, and endometriosis. You will learn that even disorders that seemingly have nothing to do with hormones, such as heart disease and osteoporosis, can be affected by a hormonal imbalance. Lastly, Part III details hormone replacement therapy, focusing on the difference between natural and synthetic hormone treatments. It explains how you can have your hormonal levels measured, and provides examples of the various hormone replacement therapies available. In addition, there is now a helpful table on the various ways to treat insulin resistance, a key factor in creating hormone imbalance.
Whether you are looking for help with menopausal symptoms or you simply want to enjoy vibrant health and well-being, this new edition of What You Must Know About Women’s Hormones can make a profound difference in the quality of your life.
Pamela Wartian Smith, MD, MPH, MS, is a diplomate of the American Academy of Anti-Aging Physicians and past co-director of the Master's Program in Medical Sciences, with a concentration in Metabolic and Nutritional Medicine, at the Morsani College of Medicine, University of South Florida. An authority on the subjects of wellness and functional medicine, she is also the founder of the Fellowship in Anti-Aging, Regenerative, and Functional Medicine. Dr. Smith is the best-selling author of ten books, including What You Must Know About Vitamins, Minerals, Herbs & So Much More; What You Must Know About Women's Hormones; and What You Must Know About Memory Loss.
"Provides a clear and concise guide to the treatments of hormonal irregularities without the health risks associated with standard hormone replacement therapy . . . [this book] can and will make a profound difference in the quality of a woman's life. Comprehensive, informative, and thoroughly 'reader friendly' in organization and presentation."
PART I: HORMONES
ESTROGEN
Anderson, B., et al., “Estrogen replacement therapy decrease hyperandrogenicity and improves glucose homeostasis: Plasma lipids in postmenopausal women with NIDDM,” Jour Clin Endorinol 1997; 82(2):638-43.
Asthana, S., et al., “Transdermal estrogen improves memory in women with Alzheimer’s disease.” Neurosci Abstr 1996; 22:200.
Bakken, K., et al., “Hormone replacement therapy and incidence of hormone-dependent cancers in the Norwegian Women and Cancer study,” Inter Jour Cancer 2004; 112(1):130-34.
Ball, P., et al., “Formation, metabolism, and physiologic importance of catecholestrogens,” Amer Jour Obstet Gynecol 1990; 163:2163-70.
Barber, D., et al., “Endothelin receptors are modulated in association with endogenous fluctuations in estrogen,” Amer Jour Physiol 1996; 271:H1999-H2006.
Barnebei, V., et al., “Plasma homocysteine in women taking hormone replacement therapy: the postmenopausal estrogen/progestin interventions in (PEPI) trial,” Jour Women’s Health Gend Based Med 1999; 8(9):1167-72.
Barrett-Conner, E., et al., “Estrogen replacement therapy and cognitive function in older women,” JAMA 1993; 269:2637-41.
Bassil, N., et al.., “Endocrine aspects of healthy brain aging,” in Desai, A., (Ed.) Healthy Brain Aging: Evidence Based Methods to Preserve Brain Function and Prevent Dementia, 2010; 26(1):57-74.
Birge, S., “The use of estrogen in older women,” Clin Geriatr Med 2003; 19(3):617-27.
Brincat, M., et al., “Sex hormones and skin collagen content in postmenopausal woman,” Brit Med Jour 1983; 287(6402):1337-38.
Brineat, M., et al., “Long-term effects of the menopause and sex hormones on skin thickness,” Brit Jour Obstet Gynecol 1985; 92(30:256-59.
Brosnan, J., et al., “Haemostatic activation in postmenopausal women taking low-dose hormone therapy: less effect than with transdermal administration?” Thromb Haemost 2007; 97:558-65.
Bruce, A., et al., “Estrogen attenuates, and corticosterone exacerbates excitotoxin oxidative injury and amyloid beta-peptide toxicity in hippocampal neuron,” Jour of Neurochem 1996; 66(5):1836-44.
Budoff, M., et al., “Effects of hormone replacement on progression of coronary calcium as measured by electron beam tomography,” Jour Women’s Health 2005; 14:410-17.
Bush, R., et al., “Cardiovascular mortality and non-contraceptive estrogen use in women: results from the Lipid Research Clinics Program follow-up study,” Circulation 1987; 75:1102-09.
Caulin-Glaser, T., et al., “Effects of 17 beta-estradiol on cytokine-induced endothelial cell adhesion molecule expression,” Jour Clin Invest 1996; 98:36-42.
Chadhurz, N., et al., “Antioxidant and pro-oxidant actions of estrogens: potential physiological and clinical implications,” Seminars Reprod Endocrinol 1998; 16(4):309-14.
Chang, K., et al., “Influences of percutaneous administration of estradiol and progesterone on human breast epithelial cell cycle in vivo,” Fertil Steril 1995; 63(4):785-91.
Chen, F., et al., “Comparison of transdermal and oral estrogen-progestin replacement therapy: effects on cardiovascular risk factors,” Menopause 2001; 8:347-52.
Chetkowski, R., et al., “Biologic effects of transdermal estradiol,” NEJM 1986; 314:1615-20.
Cohen, L., et al., “Short-term use of estradiol for depression in perimenopausal and postmenopausal women: A preliminary report,” Amer Jour Psychiatry 2003; 160:1519-22.
Colacurci, N., et al., “Effects if hormone replacement therapy on glucose metabolism,” Panminerva Med 1998; 40(1):18-21.
Compton, J., et al., “HRT and its effect on normal ageing of the brain and dementia,” Brit Jour Clin Pharmacol 2001; 52(6):647-53.
Cowan, L., et al., “Breast cancer incidence in women with a history of progesterone deficiency,” Amer Jour Epidemiol 1981; 114(2):209-17.
Crook, D., “The metabolic consequences of treating postmenopausal women with non-oral hormone replacement therapy,” Brit Jour Obstet Genecol 1997; 104(Suppl 16):4-13.
Dayas, C., et al., “Effects of chronic oestrogen replacement on stress-induced activation of hypothalmic-pituitary-adrenal axis control pathways,” Jour Neuroendocrinol 2000; 12:784-94.
Di Paolo, T., et al., “Modulation of brain dopamine transmission by sex steroids,” Rev Neurosci 1995; 5:27-41.
Drake, E., et al., “Associations between circulating sex steroid hormones and cognition in normal elderly women,” Neurology 2000; 54(3):599-603.
Dubey, R., et al., “Estradiol metabolites inhibit endothelin synthesis by an estrogen receptor-independent mechanism,” Hypertension 2001; 37:640-44.
Duckles, S., et al., “Estrogen and mitochondria: a new paradigm for vascular protection?” Mol Interv 2006; 6:26-35.
Duff, S., et al., “A beneficial effect of estrogen on working memory in postmenopausal women taking hormone replacement therapy,” Horm Behav 2000; 38(4):262-76.
Duka, T., et al. “The effects of 3-week estrogen hormone replacement on cognition in elderly healthy females,” Psychopharmacology 2000; 149(2):129-39.
Farzaneh, S., et al., “Estrogen receptor ligands: A review (2013-2015),” Sci Pharm 2016; 13:84(3):409-27.
Felson, D., et al., “Aromatase inhibitors and the syndrome of arthralgias with estrogen deprivation,” Arthritis Rhemat 2005; 52:2594-98.
Foegh, M., et al., “Estradiol inhibition of arterial neointimal hyperplasia after balloon injury,” Jour Vasc Surg 1994; 19(4):722-26.
Foidart, J., et al., “Estradiol and progesterone regulate the proliferation of human breast epithelial cells,” Fertil Steril 1998; 69(5):963-69.
Follingstad, A., “Estriol, the forgotten estrogen,” JAMA 197; 239(1):29-30.
Fournier, A., et al., “Breast cancer risk in relation to different types of hormone replacement therapy in the E3N-EPIC cohort,” Int Jour Cancer 2005; 114(3):448-54.
Fournier, A., et al., “Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study,” Breast Cancer Res Treat 2008; 107(1):103-11.
Gallagher, P., et al., “Estrogen regulation of angiotensin-converting enzyme mRNA,” Hypertension 1999; 33:323-28.
Gangar, K., et al., “Pulsatility index in internal carotid artery in relation to transdermal oestradiol and time since menopause,” Lancet 1991; 338:839-42.
Ganger, K., et al., “Pulsatility index in internal carotid artery in relation to transdermal oestradiol and time since menopause,” Lancet 1991; 338:839-42.
Garcia-Segura, L., et al., “Synaptic remodeling in arcuate nucleus after injection of estradiol valerate in adult female rats,” Brain Res 1986; 366:131-35.
Gebara, O., et al., “Association between increased estrogen status and increased fibrinolytic potential in the Framingham Offspring Study,” Circulation 1995; 91:1952-58.
Gibbs, R., et al., “Estrogen and cognition: applying preclinical findings to clinical perspectives,” Jour Neurosci Res 2003; 74(5):637-43.
Gilson, G., et al., “A perspective on HRT for women: Picking up the pieces after the Women’s Health Initiative Trial, Part I, 2003; Intern Jour Pharmaceutical Compounding,” 7(4):25-56, 277, 285-91.
Gorodeski, G., et al., “Estrogen decrease in tight junctional resistance involves matrix-metalloproteinase-7-mediated remodeling of occludin,” Endocrinology 2007; 148:218-31.
Halbreich, U., et al., “Role of estrogen in postmenopausal depression,” Neurol 1997; 48(5):516. (Suppl 7).
Head, K., “Estriol: safety and efficacy,” Alern Med Rev 1998; 3:101-13.
Henderson, B., et al., “Estrogen replacement therapy and protection from acute myocardial infarction,” Amer Jour Obst and Gyn 1988; 159:312-17.
Henderson, B., et al., “Estrogen replacement therapy and protection from acute MI,” Amer Jour Obstet Gynecol 1988; 159:312-17.
Henderson, V., et al., “Cognitive skills associated with estrogen replacement in women with Alzheimer’s disease,” Psychoneuroendocrinol 1996; 2194):421-30.
Henderson, V., et al., “Estrogen replacement therapy for the prevention and treatment of Alzheimer’s disease,” CNS Drugs 1997; 5:343-51.
Henderson, V., et al., “Estrogen replacement therapy in older women. Comparisons between Alzheimer’s disease cases and nondemented control subjects,” Arch Neurol 1994; 51(9):896-900.
Henderson, V., et al., “Postmenopausal hormone therapy and Alzheimer’s disease risk: interaction with age,” Jour Nerol Neurosurg Psychiatr 2005; 76:103-05.
Hogervorst, E., et al., “The nature of the effect of female gonadal hormone replacement therapy on cognitive function in postmenopausal women: a meta-analysis,” Neuroscience 2000; 101:485-512.
Iorga, A., et al., “Estrogen rescues heart failure through estrogen receptor beta activation,” Biol Sex Diff 2018; 9(1):48.
Iorga, A., et al., “Rescue of pressure overload-induced heart failure by estrogen therapy,” Jour Amer Heart Assoc 2016; 5(1):e002482.
Juan, S., et al., “17 beta –estradiol inhibits cyclic strain-induced endothelin-1 gene expression within vascular endothelial cells,” Amer Jour Physiol Heart Circ Physiolog 2004; 287:H1254-H1261.
Kannel, W., et al., “Fibrinogen and the risk of cardiovascular disease: the Framingham Study,” JAMA 1987; 258:1183-86.
Karim, R., et al., “Relationship between serum levels of sex hormones and progression of subclinical atherosclerosis in postmenopausal women,” Jour Clin Endocrinol Metab 2008; 93:131-38.
Kim, S., et al., “Estriol ameliorates autoimmune demyelinating disease: implications for multiple sclerosis,” Neurology 1999; 52(6);1230-38.
Krasinski, K., et al., “Estradiol accelerates functional endothelial recovery after arterial injury,” Circulation 1997; 95:1768-72.
Lauritzen, C., et al., “Results of a 5 year prospective study of estriol succinate treatment in patient with climacteric complaints,” Horm Metabol Res 1987; 19:579-84.
LeBlanc, E., et al., “Hormone replacement therapy and cognition: systemic review and meta-analysis,” JAMA 2001; 285:1489-99.
Lemon, H., et al., “Estriol prevention of mammary carcinoma induced by 7, 12-dimethyl-benzanthracene and procarbazine,” Cancer Res 1975; 35:1341-52.
Levin, E., “Integration of the extranuclear and nuclear actions of estrogen,” Mol Endocrinol 2005; 19:1951-59.
Li, L., et al., “Variant estrogen receptor-c Src molecular interdependence and c-Src structural requirement for endothelial NO synthase activation,” Proc Natl Acad Sci USA 2007; 104:16468-73.
Lieberman, E., et al., “Estrogen improves endothelium-dependent flow-mediated vasodilation in postmenopusal women,” Ann of Int Med 1994; 121:936-41.
Lobo, R., et al., “Prevention of diseases after menopause,” Climacteric 2014; 17(5):540-56.
Lopez-Jaramillo, P., et al., “Improvement in functions of the central nervous system by estrogen replacement therapy might be related with an increased nitric oxide production,” Endothelium 1999; 6(4):263-6.
Losordo, D., et al., “Variable expression of the estrogen receptor in normal and atherosclerotic coronary arteries of premenopausal women,” Circulation 1994; 89:1501-10.
Luine, V., et al., “Effect of estradiol on turnover of type A monoamine oxidase in brain,” Jour Neurochem 1977; 28:1221-27.
Luine, V., et al., “Estrogen increases choline acetyltransferase activity in specific basal forebrain nuclei and projection areas of female rats,” Experimental Neurology 1985; 80:484-90.
MacKenzie-Graham, A., et al., “Estriol-mediated neuroprotection in multiple sclerosis localized by voxel-based morphometry,” Brain Behav 2018; 8(9):e01086.
Mackey, R., et al., “Hormone therapy, lipoprotein subclasses, and coronary calcification: the Healthy Women Study,” Arch Intern Med 2005; 165:510-15.
Manolio, T., et al., “Associations of postmenopausal estrogen use with cardiovascular disease and its risk factors in older women,” Circulation 1993; 88: 2163-71.
Manonai, J., et al., “Effect of oral estriol on urogenital symptoms, vaginal cytology, and plasma hormone level in postmenopausal women,” Jour Med Assoc Thai 2001; 84:539-44.
Manson, J., et al., “Estrogen therapy and coronary-artery calcification,” NEJM 2007; 356:2591-2602.
Masuda, H., et al., “Estrogen-mediated endothelial progenitor cell biology and kinetics for physiological postsnatal vasculogenesis,” Cir Res 2007; 101:598-606.
McCrohon, J., et al., “Effects of hormone replacement therapy on the cardiovascular system,” in Estrogens and Progestogens in Clinical Practice. Fraser, J. (Eds.,) New York: Harcourt Publishers, 2000, p. 711-25.
McEwen, B., et al., “Observations in a preliminary open trial of estradiol therapy for senile dementia—Alzheimer’s type, “Psychneuroendocrinol, 1986; 11(3):337-45.
Mercuro, G., et al., “Evidence of a role of endogenous estrogen in the modulation of autonomic nervous system,” Amer Jour Cardiol 2000; 85:787-89.
Micheli, A., et al., “Endogenous sex hormones and subsequent breast cancer in premenopausal women,” Int Jour Cancer 2004; 112(2):312-18.
Miller, A., et al., “Effect of gender on NADPH-oxidase activity, expression, and function in the cerebral circulation: role of estrogen,” Stroke 2007; 38:2142-49.
Miller, V., et al., “Sex steroids and endothelial function: translating basic science to clinical practice,” Trends Pharmacol 2007; 28:263-70.
Miller, V., et al., “Vascular actions of estrogens: functional implications,” Pharmacological Rev 2008; 60(2):210-41.
Miller, V., et al., “Vascular effects of estrogen and progesterone,” in Estrogens and Progestogens in Clinical Practice. Fraser, J. (Eds.,) New York: Harcourt Publishers, 2000, p. 215-23.
Monacada, S., et al., “The L-arginine nitric oxide pathway,” NEJM 1993; 329:2002-12.
Moriarty, K., et al., “Mini review: estrogen receptor-mediated rapid signaling,” Endocrinology 2006; 147:5557-63.
Morrison, A., et al., “A prospective study of ERT and the risk of developing Alzheimer’s disease in the Baltimore longitudinal study of aging,” abstract, Neurol 1996:46:A435-6.
Morrison, J., et al., “Life and death of neurons in the aging brain,” Science, 1997; 278:412-19.
Mueck, A., et al., “Comparison of the proliferative effects of estradiol and conjugated equine estrogens on human breast cancer cells and impact of continuous combined progestogen addiction,” Climacteric 2003; 6(3):221-27.
Murkes, D., et al., “Effects of percutaneous estradiol-oral progesterone versus oral conjugated equine estrogens-medroxyprogesterone acetate on breast cell proliferation and bel-2 protein in healthy women,” Fertil Steril 2011; 95(3):1188-91.
Murkes, D., et al., “Percutaneous estradiol/oral micronized progesterone has less-adverse effects and different gene regulations than oral conjugated equine estrogens/medroxyprogesterone acetate in the breast of healthy women in vivo,” Gynecol Endocrinol 2012; 28(Suppl 2):12-5.
Na, K-S., et al., “The ocular benefits of estrogen replacement therapy: a population-based study in postmenopausal Korean women,” PLoS One 2014; 9(9):e106473.
Nabulsi, A., et al., “Association of hormone-replacement therapy with various cardiovascular risk factors in postmenopausal women,” NEJM 1993; 328:1069-75.
Nachtigall, L., et al., “Serum estradiol-binding profiles in postmenopausal women undergoing three common estrogen replacement therapies: Associations with sex hormone-binding globulin,
estradiol, estrone levels,” Menopause 2000; 7:243-50.
Naftolin, F., et al., “Cardiovascular health and the menopausal woman: the role of estrogen and when to begin and end hormone treatment,” F1000 Res 2019; PMID 31543950.
Neubauer, H., et al., “Overexpression of progesterone receptor membrane component 1: possible mechanism for increased breast cancer risk with norethisterone in hormone therapy,” Menopause 2013; 20(5):504-10.
Nickenig, G., et al., “Estrogen modulates AT1 receptor gene expression in vitro and in vivo,” Circulation 1998; 97:2197-2201.
Novella, S., et al., “Vascular aging in women: Is estrogen the fountain of youth?” Front Physiol 2012; 3:165.
Novensa, L., et al., “Equine estrogens impair nitric oxide production and endothelial nitric oxide synthase transcription in human endothelial cells compared with the natural 17(beta)-estradiol,” Hypertension 2010; 56(3):405-11.
O’Keefe, J., et al., “Estrogen replacement therapy after coronary angioplasty in women,” Amer Coll Cardiol 1997; 29(1):1-5.
O’Lone, R., et al., “Estrogen receptors alpha and beta mediate distinct pathways of vascular gene expression, including genes involved in mitochondrial electron transport and generation of reactive oxygen species,” Mol Endocrinol 2007; 21:1281-96.
Ohkura, T., et al., “ERT for dementia of the Alzheimer type in women,” in Berg, G., et al., (Eds.), The Modern management of the Menopause. Proceedings of the VII International Congress on the Menopause. Stockholm, Sweden. London, NY: Parthenon Publishing Group, 1993; p. 315-33.
Ospina, J., et al., “17B-estradiol decreases vascular tone in cerebral arteries by shifting COX-dependent vasoconstriction to vasodilation,” Amer Jour Physiol Heart Circ Physiol 2003; 285:H241-H250.
Ottosson, U., et al., “Oral progesterone and estrogen/progestogen therapy, effects of natural and synthetic hormones on subfractions of HDL cholesterol and liver proteins,” ACTA Obstet Gynecol Scand 1984; (Suppl):127-37.
Paganini-Hill, A., et al., “Alzheimer’s disease in women,” The Female Patient 1998; 23:10-20.
Paganini-Hill, A., et al., “Does estrogen replacement therapy protect against Alzheimer’s disease? Osteoporosis Int 1997; Supp 1:S12-17.
Paganini-Hill, A., et al., “Estrogen deficiency and risk of Alzheimer’s disease in women,” Amer Jour Epidemiol 1994; 140:256-61.
Paganini-Hill, A., et al., “Estrogen replacement therapy and risk of Alzheimer’s disease,” Arch Int Med 1996; 156(19):2213-17.
Panossian, A., et al., “Evidence-based efficacy of adaptogens in fatigue, and molecular mechanisms related to their stress-protective activity,” Curr Clin Pharmacol 2009; 4(3):198-219.
Pansini, F., et al., “Control of carbohydrate metabolism in menopausal women receiving transdermal estrogen therapy,” Ann NY Acad Sci 1990; 592:460-62.
Patel, S., “Estrogen: The necessary evil for human health, and ways to tame it,” Biomed Pharmacother 2018; 102:403-11.
Phillips, S., et al., “Effects of estrogen on memory function in surgically menopausal women,” Psycho Neuroendo 1992; 17(5):485-95.
Poehlman, E., et al., “Changes in energy balance and body composition at menopause: A controlled longitudinal study,” Ann Int Med 1995; 123(9):673-75.
Prelevic, G., et al., “The effect of oestrogen and progestogen replacement therapy on systolic flow velocity in healthy postmenopausal women,” Maturitas 1994; 20:37-44.
Proudler, A., et al., “Hormone replacement therapy and serum angiotensin-converting-enzyme activity in postmenopausal women,” Lancet 1995; 346:89-90.
Puder, J., et al., “Estrogen modulates the hypothalamic-pituitary-adrenal and inflammatory cytokine responses to endotoxin in women,” Jour Clin Endocrinol Metab 2001; 86(6):2403-08.
Raz, R., et al., “A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections,” NEJM 1993; 329:753-56.
Richman, S., et al., “Low-dose estrogen therapy for prevention of osteoporosis: working our way back to monotherapy,” Menopause 2006; 13(1):148-55.
Rocca, W., et al., “Increased risk of cognitive impairment or dementia in women who underwent oophorectomy before menopause,” Neurology 2007; 69(11):1074-83.
Rosano, G., et al., “Syndrome X in women in associated with estrogen deficiency,” Eur Heart Jour 1995; 16:610-14.
Salpeter, S., et al., “Bayesian meta-analysis of hormone therapy and mortality in younger postmenopausal women,” Amer Jour Med 2009; 22(11):1016-22.
Sarrel, P., et al., “Ovarian hormones: recent findings of cardiological significance,” Cardiol Pract 1991; Mar-Apr, p. 14-17.
Sarrel, P., et al., “The mortality toll of estrogen avoidance: An analysis of excess deaths among hysterectomized women aged 50 to 59 years,” Amer Jour Public Health 2013; 103(9):1583-88.
Scoccianti, C., et al., “Female breast cancer and alcohol consumption: a review of the medical literature,” Amer Jour Prev Med 2014; 46(3 Suppl 1):S:16-25.
Scoccianti, C., et al., “Recent evidence on alcohol and cancer epidemiology,” Future Oncol 2013; 9(9):1315-22.
Seed, M., et al., “The effect of hormone replacement therapy and route of administration on selected cardiovascular risk factors in post-menopausal women,” Fam Pract 2000; 17:497-507.
Shaywitz, S., et al., “Effect of estrogen on brain activation patterns in postmenopa ...